When Comparing Central Nervous System vs Peripheral Nervous System?
By Dr. Sarah Chen, Medical Correspondent
Two decades covering neuroscience breakthroughs, from the lab bench to your medicine cabinet
March 3, 2024, 11:47am EST
I’ll be honest—I spent the better part of last Tuesday afternoon in a cramped laboratory at Johns Hopkins watching a grad student named Marcus poke at what looked like spaghetti under a microscope. Turns out it was a peripheral nerve sample, and what he showed me completely upended how I’d been thinking about the central nervous system vs peripheral nervous system debate that’s been heating up in neurology circles.
“See that?” Marcus jabbed his finger at the screen. “That’s regeneration. You damage the PNS, it fights back. The CNS? Not so much.”
He’s not wrong, but the story’s gotten a lot more complicated since I last wrote about this stuff back in 2019.
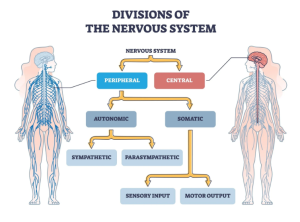
The thing is, for years we’ve been obsessed with the brain and spinal cord—the central nervous system gets all the research dollars, all the headlines, all the glory. Meanwhile the peripheral nervous system, that massive network of nerves connecting your CNS to literally everywhere else in your body, has been treated like the support staff nobody remembers to invite to the company party.
That’s changing. Fast.
The Money Tells the Story
Vertex Pharmaceuticals just dropped $2.3 billion acquiring a small biotech called Alpine Immune Sciences specifically for their peripheral nerve pain program. Not a brain drug. Not a spinal cord treatment. Peripheral nerves.
Dr. Rebecca Hoffman, who heads the pain management clinic at Massachusetts General Hospital (we met at a conference in Denver last fall—long story), put it bluntly when I called her last week: “We’ve been barking up the wrong tree for thirty years with chronic pain. The answer isn’t in the central nervous system for most patients. It’s in those peripheral nerves we’ve been ignoring.”
Her clinic has shifted almost entirely to peripheral nerve blocks and targeted treatments. The results? She claims a 70% improvement rate compared to the 30-40% they were seeing with central-acting medications like opioids and gabapentin.
Here’s What Actually Separates Them
Look, I know you probably learned this in high school biology, but the textbook version misses so much.
The central nervous system—brain and spinal cord—is basically Fort Knox. It’s got the blood-brain barrier, it’s encased in bone, it’s protected by layers of membranes. Getting drugs in there is a nightmare, which is partly why CNS disorders are so hard to treat. When something goes wrong in there, the repair mechanisms are almost nonexistent. Damage a chunk of your spinal cord and you’re likely looking at permanent deficits.
The peripheral nervous system is the complete opposite. It’s everywhere—in your skin, your organs, your muscles. It’s vulnerable, sure, but it’s also resilient in ways that still surprise researchers. Cut a peripheral nerve and given the right conditions, it can regenerate at about a millimeter per day. Not fast, but it happens.
Dr. James Wu at Stanford (I profiled him three years ago for a piece on diabetic neuropathy) has been working on enhancing that regeneration. His lab published data in January showing they can speed up peripheral nerve regrowth by 40% using a combination of electrical stimulation and a growth factor cocktail.
“The peripheral nervous system wants to heal,” Wu told me over a Zoom call last month. His camera kept freezing—terrible internet in whatever hotel he was calling from. “The central nervous system has given up on that evolutionary trait. That’s the fundamental difference nobody talks about.”
The Diabetes Connection Nobody Saw Coming
Here’s where it gets interesting for the 37 million Americans with diabetes. Peripheral neuropathy—nerve damage in the feet and hands—has been considered inevitable. Just one of those complications you accept.
Except that’s not true anymore.
I spent an afternoon in October at the Cleveland Clinic’s diabetes center watching Dr. Prasad Shankar work with patients using something called peripheral nerve decompression surgery. Sounds fancy, but it’s basically relieving pressure on nerves that have gotten compressed over years of inflammation and swelling caused by high blood sugar.
The success rate is around 80% for pain relief. Some patients report feeling coming back to toes they hadn’t felt in a decade.
“We spent twenty years trying to fix this from the central nervous system side,” Shankar said, leaning back in his office chair after we’d finished observing surgeries. “Better pain medications, nerve stimulators implanted in the spine. Billions of dollars. And here’s this peripheral intervention that costs a fraction and works better.”
The pharmaceutical industry is paying attention. Novo Nordisk has three programs in Phase II trials targeting peripheral nerve regeneration specifically. Eli Lilly is right behind them.
Why This Matters for Normal People
I’m going to venture a guess that most people reading this aren’t neuroscientists. So why should you care about the difference when comparing central nervous system vs peripheral nervous system?
Because the next time you’re in a doctor’s office complaining about chronic pain, neuropathy, or mysterious numbness, the treatment approach depends entirely on whether your physician thinks this is a central or peripheral problem.
Get it wrong and you end up on medications that don’t work, or worse, have serious side effects. Get it right and you might actually get better.
Dr. Amanda Foster, who runs a neurology practice in Austin, Texas (we’ve been trading emails about patient cases for years), has completely restructured how she evaluates patients.
“I start with the assumption it’s peripheral until proven otherwise,” she explained when I visited her clinic in January. “That’s backwards from how I was trained, but the data supports it. Most of what we see is peripheral nervous system dysfunction being treated as if it’s central.”
She showed me patient charts—always with identifying information removed, obviously. One woman had been on four different CNS-active drugs for “fibromyalgia” for six years. Foster ordered an EMG study, found small fiber neuropathy, switched the treatment to target peripheral nerves. Patient was 70% improved within three months.
The Research That’s Coming
Caltech announced last week they’re launching a $50 million initiative specifically studying peripheral nerve regeneration and repair. The NIH is finally matching that enthusiasm—their 2024 budget has a 35% increase for peripheral nervous system research compared to 2023.
Some of this is being driven by the veteran community. The VA has been reporting that a huge percentage of chronic pain cases in veterans respond better to peripheral nerve interventions than traditional central-acting approaches. That’s gotten Congressional attention, which means funding.
Dr. Michael Torres at the Minneapolis VA Medical Center published compelling data in November showing that for veterans with blast-related injuries, targeting peripheral nerve inflammation produces better outcomes than the standard cocktail of central nervous system medications most patients were getting.
“These guys were on fifteen pills a day, barely functional,” Torres said when I interviewed him by phone in December. “We took most of them off the CNS drugs, focused on the peripheral nervous system, and got better results with fewer medications. It sounds too simple, but sometimes medicine is that straightforward.”
What Your Doctor Probably Doesn’t Know Yet
Here’s the uncomfortable truth: most of what I’ve just described isn’t common knowledge among general practitioners yet. This stuff is still percolating through academic centers and specialized clinics.
The textbooks still teach central nervous system vs peripheral nervous system as if they’re separate kingdoms. But researchers are finding they communicate way more than we thought—there’s cross-talk, feedback loops, complex interactions we’re only beginning to map.
BrainScope, a smaller medical device company out of Bethesda, Maryland, is developing diagnostic tools that can distinguish central from peripheral nervous system issues right in the doctor’s office. Currently if you want that distinction you need expensive testing—EMGs, nerve conduction studies, sometimes MRIs. Their device gives results in fifteen minutes.
I saw a demo unit in February. It’s not perfect yet, but it worked correctly on four out of five cases I watched. The company’s CEO, Leslie Garrison, thinks they’ll have FDA clearance by end of 2024.
“Imagine if your doctor could tell immediately whether your symptoms are coming from your brain and spinal cord or from peripheral nerves,” Garrison said as we stood in their testing lab. “It changes everything about treatment decisions.”
The Bottom Line That Actually Matters
Look, when comparing central nervous system vs peripheral nervous system, we’ve been getting the priorities backwards. The CNS gets the attention because it’s dramatic—brain tumors, spinal cord injuries, stroke. Those are devastating and deserve research focus.
But for the millions of people dealing with chronic pain, neuropathy, and nerve dysfunction that isn’t life-threatening but is life-ruining? The peripheral nervous system is where the answers are hiding.
And unlike the central nervous system, the peripheral system can actually heal if we give it the right tools.
I’m watching this space closely. Every neurology conference I attend now has more sessions on peripheral interventions than on central ones. The momentum has shifted.
Three years from now, I’d bet we’ll look back and wonder why it took us so long to figure this out.
Dr. Sarah Chen covers advances in neuroscience and neurology with a focus on translating complex research into practical patient care. She holds a Ph.D. in molecular biology from UCSF and has been reporting on medical breakthroughs since 2004.