Can you list characteristics of the pns?
Neurology Research Associate March 2024
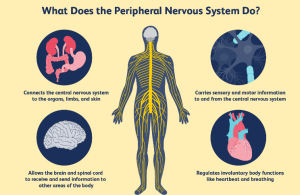
So here’s the thing about the peripheral nervous system that always gets me when I’m trying to explain it to med students – it’s basically everything that’s NOT your brain and spinal cord, which sounds simple until you realize how ridiculously complex that actually is.
I remember during my residency, one of my attendings used to say the PNS was like the “wiring harness” of a car, except that analogy falls apart pretty quick because car wiring doesn’t regenerate itself or adapt based on what you’re doing. But whatever, it stuck with me.
The Basic Setup (Sort Of)
The peripheral nervous system’s got this dual personality thing going on. There’s the somatic part – that’s your voluntary movement and sensation stuff – and then the autonomic part, which handles all the background processes you don’t think about. Like, right now your heart’s beating and you’re digesting lunch (or should be eating lunch if you’re reading this at 2pm like I usually do), and none of that requires conscious effort.
The cranial nerves are technically part of the PNS even though they emerge from the brainstem. Twelve pairs of them. I still use that ridiculous mnemonic from med school to remember their order, the one that’s too inappropriate to print here. But honestly? In practice, you mostly worry about the vagus nerve (that’s number X) because it does SO much – controls heart rate, digestion, even affects mood through the gut-brain axis that everyone’s obsessed with lately.
Regeneration: The Plot Twist
Here’s where it gets interesting, and why peripheral nerve injuries aren’t always permanent like CNS damage typically is. PNS neurons can actually regenerate. Not quickly – we’re talking maybe 1mm per day under ideal conditions – but they CAN do it. I had a patient last year who severed the median nerve in his wrist (nasty table saw accident, don’t ask), and over about 8 months he gradually got sensation and motor function back. Not perfect, mind you. Never quite perfect with these injuries.
The Schwann cells are the MVPs here. They form the myelin sheaths around peripheral nerve axons, and when there’s damage, they create this guidance channel situation that helps the nerve fiber find its way back. It’s called a Band of Büngner if you want to get technical, named after some 19th-century German guy who probably had an impressive mustache.
CNS myelin is formed by oligodendrocytes instead, and they’re nowhere near as helpful when things go wrong. That’s part of why spinal cord injuries are so devastating.
The Autonomic Drama
The autonomic nervous system splits into sympathetic and parasympathetic divisions, and they’re basically frenemies. Sympathetic is your “fight or flight” response – pupils dilate, heart races, digestion stops because who needs to process food when you’re running from a bear? (Even though the last time most of us ran from anything was probably to catch a bus.)
Parasympathetic is “rest and digest.” Slows heart rate, stimulates digestion, constricts pupils. The vagus nerve I mentioned earlier? That’s parasympathetic, and it’s weirdly become trendy in wellness circles lately. “Vagal tone” this, “stimulate your vagus nerve” that. Some of it’s legit science, some of it’s… let’s say optimistic.
There’s also the enteric nervous system in your gut wall, which some people call the “second brain.” It’s got more neurons than your spinal cord – around 500 million – and can operate semi-independently. That “gut feeling” you get? There’s actual neural basis for that, not just metaphor.
Sensory Weirdness
The PNS handles all sensation from your skin, muscles, joints, and organs. But it’s not just “touch, temperature, pain” like they teach in intro bio. There are all these specialized receptors – Merkel cells, Pacinian corpuscles, Ruffini endings, Meissner’s corpuscles. Each responds to different stimuli.
Pacinian corpuscles, for instance, detect vibration. They’re onion-shaped (seriously, look at them under a microscope) and they’re why you can feel your phone buzzing in your pocket even through fabric. Meissner’s corpuscles are concentrated in your fingertips and lips, which is why those areas are so sensitive to light touch.
The pain pathway is its own rabbit hole. Fast pain travels via A-delta fibers at around 20 m/s – that’s the sharp, immediate “OW” when you stub your toe. Slow pain uses C fibers crawling along at maybe 2 m/s, which gives you that dull, throbbing ache afterward. Different fibers, different neurotransmitters, different brain regions they ultimately activate.
Clinical Reality Check
In neurology practice, peripheral neuropathy is everywhere. Diabetes is the usual culprit – high blood sugar damages the small blood vessels that feed peripheral nerves, starting with the longest ones (feet and legs first). That’s why diabetic patients lose sensation in their toes and feet, which then leads to ulcers they don’t feel, which can get infected, which… yeah, it’s a cascade.
But there’s also alcoholic neuropathy, chemotherapy-induced neuropathy, vitamin B12 deficiency neuropathy, autoimmune neuropathies like Guillain-Barré syndrome (where your immune system attacks myelin), hereditary neuropathies like Charcot-Marie-Tooth disease. The list goes on.
Carpal tunnel syndrome? That’s median nerve compression at the wrist – a PNS issue. Sciatica? Usually compression of nerve roots as they exit the spine, which is technically where CNS transitions to PNS.
The Coordination Problem
What still fascinates me after all these years is proprioception – your sense of where your body parts are in space without looking. Close your eyes and touch your nose. You can do it (unless you’re drunk, which is actually how we test cerebellar function, but I digress). That’s proprioceptive sensors in your muscles, tendons, and joints constantly sending position data through the PNS to your brain.
When this system breaks down – say, from a peripheral neuropathy or a spinal cord lesion – people develop sensory ataxia. They can still move, but without visual feedback they’re clumsy and uncoordinated. It’s like trying to type on a keyboard you can’t see or feel.
Development and Adaptation
During development, the PNS grows out from the neural crest and neural tube in this incredibly choreographed process. Growth cones on the end of extending axons follow chemical gradients to find their targets. Sometimes they get it wrong – there are documented cases of people with crossed wiring where touching one body part produces sensation in another location. Usually it’s acquired after injury during nerve regeneration, not developmental, but still weird.
The system’s also more plastic than we used to think. Phantom limb sensation after amputation, for example, involves reorganization of cortical maps, but the peripheral nerves are still sending confused signals from the stump. Sometimes touching the face produces sensations in the phantom hand because those cortical regions are adjacent and can take over freed-up territory.
Random Facts That Didn’t Fit Elsewhere
Your PNS nerve fibers are bundled into nerves, which are bundled into nerve trunks, all wrapped in layers of connective tissue (endoneurium, perineurium, epineurium – because anatomists love giving everything names). This layered structure provides protection but also creates compartments, which matters when you get nerve swelling or bleeding.
The blood-nerve barrier is less tight than the blood-brain barrier, which is why peripheral nerves are more vulnerable to circulating toxins and why many chemotherapy drugs cause neuropathy.
Some peripheral nerves are ridiculously long. The sciatic nerve can be over a meter in tall individuals. That’s a single neuron with an axon stretching from your lower spine to your foot. Think about the metabolic challenges of keeping that alive – proteins synthesized in the cell body have to be transported all that distance.
Anyway, that’s probably more than you wanted to know about PNS characteristics. The short version: it’s everything neural outside your brain and spinal cord, it can regenerate (slowly), it has somatic and autonomic divisions, and when it breaks down you get all sorts of clinical problems. But the long version is way more interesting, obviously.